Cowper’s Cut 277: The NHS Long-Term Workforce Plan: trolling as public policy?

The NHS Long-Term Workforce Plan: important in theory, uncertain and unclear in practice
It's arrived. Better late than never?
In hilarious launch conditions, where the PR responses of consulted and less-consulted organisations made it brutally clear that they hadn't been shown the final document (I did mention that May slide deck last week), and with a six-page, 4,500-word press release, we finally got to see The NHS Long-Term Workforce Plan - or to give it a better title, 'I Contain Multitudes' (See book 51).
PM Rishi 'The Brand' Sunak gave an awkward presser for the launch: here's the speech.
'But is The ICM Plan any good?'
"Without concerted and immediate action, the NHS will face a workforce gap of more than 260,000–360,000 staff by 2036/37".
But is the 'I Contain Multitudes' Plan any good?
Mmmmmmmmm. I recommend this fairly positive review by staffing and workforce expert Professor Alison Leary in BMJ as a starting point.
NHS England chief executive Amanda Pritchard's introduction states that The ICM Plan "doesn’t just herald the start of the biggest recruitment drive in health service history, but also of an ongoing programme of strategic workforce planning – something which is unique amongst other health care systems with national scale".
That doesn't seem to be wrong. There is a value to having this first iteration of an NHS workforce plan. Chancellor Jeremy Hunt deserves credit for overcoming Treasury Munchkins' resistance (long revealed by both himself and Simon Stevens) to any such doubtless-cost-inflationary thing.
Likewise, the commitment to update and iterate The ICM Plan is both necessary and sensible.
However, that's not saying much - which can fairly be taken as a tribute to The ICM Plan itself. Because over its 150 pages, split into thematic lumps of 'train', 'retain' and 'reform', it likewise manages not to say much.
Yes, there are numerical commitments to a doubling of medical school training places to 15,000 (some of which rise was already planned) and to increase the number of GP training places by 50% to 6,000 by 2031-32.
However. The new allocated funding over the next five years of £2.4 billion if distributed equally (which it won't be) represents about £0.5 billion a year: that is about 0.3% of the current NHS budget.
(The distinction between costs of training and the cost of the workforce expansion are likely lost on the public, and indeed on most national journalists.)
The ICM Plan promises an increase of approximately 65% in the size of the NHS workforce in 14 years time.
If we assume that the inflation rate is 2.5% over that period, and that we match inflation and don’t continue to inflict progressive sub-inflationary pay (and no real-terms pay rises), then it is something like 65 x 1.65 x (1.025)^14, which is to say a circa £150 billion wage bill in 14 years' time (assuming the same broad pay structures, which is a big assumption).
For wage expenditure to grow from £65 billion now to £150 billion by 2037 would involve wage bill growth year-on-year of about 6.5% over 14 years. Consider this, setting these approximations against recent NHS year-on-year average growth of 3.6% (although clearly we can't know future NHS average growth, particularly not over 14 years).
Is this (short of robbing the capital expenditure budget and running the NHS out of collapsed buildings and tents, and prescribing home-grown leaches) likely to happen?
The other option is that we assume that we’re not going to pay this expanded workforce very much at all.
But with no credible, detailed plan of how you treat those new staff well enough so that one in four the trainee nurses don’t leave in the first three years (as currently) and nearly 6% of them don’t go off sick every day, is it credible that this will redress the recruitment and retention crisis within a current workforce of 1.4 million people, whose salaries together account for 65% of the £160 billion of healthcare expenditure?
The headline promise on 'retain' is that "by improving culture, leadership and wellbeing, we will ensure up to 130,000 fewer staff leave the NHS over the next 15 years". Mmmmmmmmmmm for maybe.
Particularly because there is no evidence that NHS England is nor can become any good at improving any of these things.
A quick thought on culture and change: remember the ambitious, bright group of younger NHS managers and management trainees who oversaw and ran the original iteration of NHS Change Day (before its capture by the corporate, the egotistical and the flaky), or who made and maintained online collaboration platforms (long before integration and collaboration were in policy vogue).
How have those people been valued? Where are they now?
The 'reform' section will alarm and inflame those already concerned that this is about replacing high-training, high-skill professions with cheaper, lower-skilled options.
These people seem unlikely to be reassured by its promises/threats that "working differently means enabling innovative ways of working with new roles as part of multidisciplinary teams so that staff can spend more time with patients. It changes how services are delivered, including by harnessing digital and technological innovations. Training will be reformed to support education expansion".
The reality is that junior doctors are already getting less training than would be ideal almost everywhere, and are being extensively used 'on take'; as manager-substitutes; or as pseudo-IT staff (among many consultants' concerns about doing strike cover was that only the juniors know how to work EPR systems).
How will extra senior staff time be found to train more, or properly? The ICM Plan does not say (but it'll probably be down to AI).
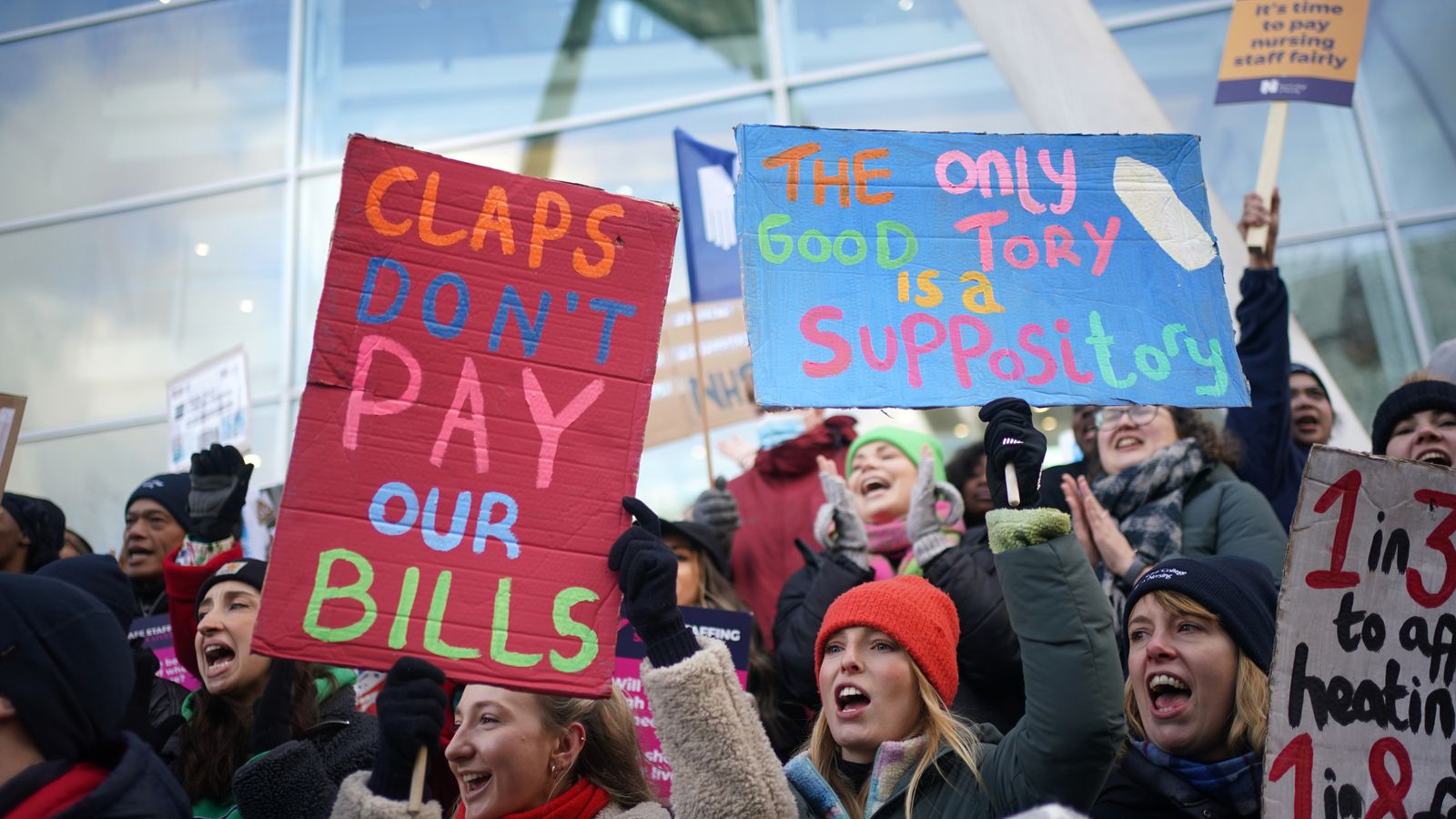
It was a bitter irony that as The ICM Plan was being announced, radiographers voted to join the current waves of pay strikes: more of which below.
The BBC's Laura Kuennsberg Show featured an interview with Amanda Pritchard channeling her inner Chris Hopson, and with scintillating Secretary Of State For The Next Fifteen Months Steve 'The Banker' Barclay. There wasn't much positive message for either NHS staff or for patients from either: Amanda did manage to say of the ongoing strikes that "it is patients that are paying the price for the fact that all sides have failed to reach a resolution".
This, of course, ignores the fact that it costs NHS clinicians money to strike.
Political consequences
The ICM Plan has nicked Labour's plan to double training places, and Mr Barclay committed on Kuennsberg that the £2.4 billion (inadequate as it is) will be new cash in the forthcoming Budget.
This going into the NHS funding baseline gives Labour back the £3 billion from ending non-dom tax status that they were going to spend on this.
Labour health lead Wes Streeting's brief Sunday Times 'what I'd do' piece repays reading.
A bit of good news
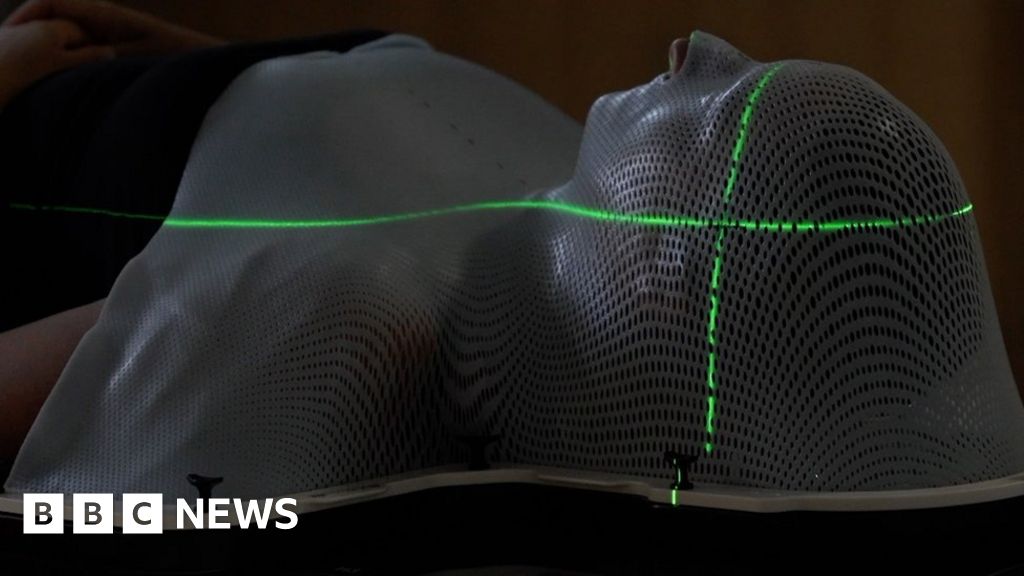
By contrast, this is a nice story on BBC News about actual use of parttern recognition software (AI, if you must). Researchers at Addenbrooke's Hospital trained this 'AI' program with Microsoft: it helps doctors calculate where to direct the therapeutic radiation beams, to kill cancerous cells while sparing as many healthy ones as possible.
Sloman headlines Glastonbury
NHS England chief operating officer Sir David Sloman headlined Glastonbury.
Wow.
Meanwhile, ...
DHSC refused to use the “D word” and attempt any of things that might have mitigated. Health care workers should have been immediately seen as front line disaster responders and treated as such - fast tracked treatment, protection from moral injury, enhanced ts,cs and rest, pay!
— Professor Lucy Easthope (@LucyGoBag) June 29, 2023
Remarkable remarks on the Fictional Forty
There is a genuinely remarkable intervention by Natalie Forrest, the Department For Health But Social Care's head of the New If Fictional Hospitals Programme in this interview with Health Service Journal.
She says that "there shouldn’t be a special group that are getting rebuilt, and everyone else has to watch from the sidelines. Building new hospitals should be like painting the Forth Bridge – it should never stop ... we want a pipeline not a flurry of 40 at once”.
(The NIFHP director even went so far as to defy all NHS tradition and assert that "you shouldn’t have to campaign to get a new hospital”.)
In other words, Forrest makes it crystally clear that the Fictional Forty (later Forty-Eight) New Hospitals claim that was a 2019 Conservative And Unionist Party manifesto pledge is obviously nonsense.
Ahem. Oh, did I mention this was nonsense back in 2019, I hear you ask? Why yes, indeed I did: thank you for asking.
This sort of lese-mejeste intervention doesn’t happen with a Government manifesto commitment, unless that Government is obviously about to lose a General Election very heavily indeed.
With heroic optimism on both basic organisational capacity and capital availability, Forrest adds, "what we don’t want is for us to have to stop building hospitals because it’s not on anyone’s political agenda. It should be what we do. That’s why it needs to be driven by the NHS". Bless.
In an heroically tardy bit of timing, YouGov polled public opinion on what constitutes a "new hospital": a massive 6% of those surveyed agreed with the Government’s definition. 92% of those polled said that “a whole new hospital built from scratch on a site which previously did not contain a hospital” would come under their definition of ‘new hospital’.
14% consider “adding a major new clinical building or new wing to an existing hospital, containing a whole clinical service such as maternity or children's services” to constitute a new hospital, while 20% say the same of “a complete or major refurbishment of an existing hospital”. (As many as 78% and 72% respectively say that these projects would not count as a new hospital.)
Conservative voters are the same as the wider population in terms of their definition of a new hospital.
If you too would like to join @SAHealth with attractive lifestyle, remuneration, relocation assistance, head to https://t.co/w7Zst7UQsV
— Chris Picton MP (@PictonChris) June 27, 2023
Looking at the impact of the ongoing pay disputes (of which more below) and the rising issuing of GMC certificates of good standing, it's starting to feel as if the Government pledged to build 40 new hospitals, but just didn't mention that they'd be in Australia, New Zealand, India, Germany, America ...
So why work in NZ? Well, we understand the important difference between Wellbeing & rocks.https://t.co/GENOFASi9L
— Alex Psirides (@psirides) June 29, 2023
Industrial action
Doctors' strikes are a symptom of burnout says former NHS hospital chair@SirTomHH on senior doctors voting in favour to strike over pay next month.#KayBurley LH pic.twitter.com/3bRileK40t
— Kay Burley (@KayBurley) June 28, 2023
Big news of the week: BMA consultants voted to strike by 86% on a 71% turnout.

The inevitable 'Downfall' video has dropped.
My guess of a 60% margin for action was quite a bit too low: I underestimated the strength of feeling, and overweighted the 'consultants won't strike' anecdata.
It is, in part, about pay erosion - which is driving highly skilled and experienced doctors away in droves. It is also about staff shortages, overwhelming pressure to fix a mess not of our making, and the moral harm in providing a level of care that it is hard to be proud of.
— Professor Claire Hopkins (@SnotSurgeon) June 29, 2023
This eloquent Twitter thread by Professor Claire Hopkins explpains what I suspect is mainstream consultant thinking as to why they are acting.
(Public health consultants voted for action by the same margin, but the turnout of just 39% means their action cannot proceed.)
The heir to the toffee fortune proved that his political and people anetennae are just as bad as they ever were.
Am I alone in thinking it is wrong for consultants to strike? Nurses, paramedics, junior doctors, yes, they are just ‘workers’ but consultants are senior leaders, just like senior managers. They demean themselves by striking.
— Stephen Thornton (@Thornton_health) June 29, 2023
Absent a serious pay offer from Government (which pretty clearly won't be forthcoming), BMA consultants are set to walk out on 20 and 21 July, immediately after the five-day junior doctors' stoppage. The NHS waiting lists that the PM pledged to reduce are going to rocket yet further. "To infinity, and beyond!"

The Boris Johnson Fanzine was briefed by Team Barclay that the independent pay review body recommends a £1,000 consolidated payment to end the strikes and a 6% pay rise for the next financial year.
Mr Barclay is reportedly "minded to accept" this proposal. I’m pretty sure that the BMA junior doctors won't be.
Good old Helen Whateley: she always makes things better.
She claimed on LBC that “we have made real progress in bringing down some of the longer waits that have developed following the pandemic”. Alas, poor Helen's assertion is not true. Back here in The Real World, we know using data that even before the pandemic, NHS waits were at the highest level (then) yet recorded.
Still, they say that God loves a trier. And Ms Whateley is very trying indeed.

The RCN failed to get over the required 50% response threshold in its ballot for further (and national) strike action, so they are out of the industrial action game for the time being.

Among the causes of the industrial action is staff dissatisfaction with their working lives, as reflected in the Nuffield Trust data analysis shared with the BBC, showing that "staff sickness in the NHS in England has reached record levels. 2022 figures show an absence rate - the proportion of days lost - of 5.6%, meaning the NHS lost the equivalent of nearly 75,000 staff to illness.
"This is higher than during the peak pandemic years of 2020 and 2021 - and a 29% rise on the 2019 rate.
"Mental health problems were the most common cause, responsible for nearly a quarter of absences ... big rises were also seen in cold, coughs, infections and respiratory problems, likely to be linked to the continued circulation of Covid as well as the return of flu last year".
Poll tracks
Labour leads the Tories (in %) on nearly all policy areas, @IpsosUK poll @EveningStandard:
— Nicholas Cecil (@nicholascecil) June 27, 2023
Managing economy, by 29/24
Cost of living, 37/15
Education, 32/17
Housing, 38/11
Healthcare, 41/11
Taxation, 31/22
Asylum/immigration, 26/17
Future EU ties, 29/21 https://t.co/Wk4U1rpkQm
New polling by Ipsos for the Evening Standard finds that Labour lead the Conservatives on perceptions of those polled on almost every major public policy issue. (The Tories lead on defence alone.)
The Standard write-up says that "the top issues that people suggest they will vote on are the NHS (31 per cent), inflation/cost of living (31 per cent), managing the economy (22 per cent), asylum and immigration (15 per cent), and education (12 per cent), with just five per cent now citing Brexit/Europe which was the highest in 2019".
If there is a significant win by #Labour this will be a key part of the story - although unlike 1997, concern about #NHS is much lower - the economy dominates pic.twitter.com/MhmKWfwv4y
— Ben Page (@benatipsos) June 28, 2023
The polling data is here.
Prevention of Steve 'The Banker' Barclay
Argues that prevention is the only way to bend the demand curve, and that must mean giving people more responsibility, choice and incentives
— Robert Colvile (@rcolvile) June 27, 2023
It almost feels cruel to mock a man of the steadfast dullness of Secretary Of State For The Next Fifteen Months Steve 'The Banker' Barclay. But he will insist on giving speeches, so he's fair game.
The latest effort (summarised here, and the full text here) was titled 'A Conservative Vision For Prevention', in which The Banker exhorts the NHS to double down on giving people more control over their care.
Eh? I mean, that's probably a good thing, provided adequate educational and peer support resources are provided to help them understand the options. But it's not in any way an approach to prevention.
The Conservative vision for prevention seems to be Samuel Smiles’ ‘Self-Help; With Illustrations Of Character And Conduct’. This is likely to resonate with few in the public health community; there is also very little evidence that it works.
The People's Steve seems to advocate prevention via allowing the great British public to continue not to exercise and to eat all the lard they want, because “belief in personal freedom”. It's a novel version of prevention, I suppose.
At one point, he asserts that "too often, prevention has been dominated by the ideas of the political left. That shouldn’t be the case. And I am truly excited by the opportunities that technology and innovation are presenting to recast prevention from a Conservative perspective".
Ahem.
He also asserts that "we’re using technology to end the 8 am rush for GP appointments". This is untrue: they have issued press releases about this, which is not the same as doing it.
There are brighter doormats than Steve Barclay (which, coincidentally, are also far more useful).
He goes on to say, "most agree that prevention is the only way to bend this demand curve, but what I believe is that the only way we can do this is by giving people the tools to take more responsibility for their own health".
Does The Banker bring evidence for his belief?
You may be astonished to hear that he does not.
He further asserts "Labour seek universal models for prevention, seeing comfort in one size fits all solutions – even if this leads to poorer outcomes. That is why they often seek to tax and ban. Thinking that helping a few, justifies making everyone else comply". If it occurs to The Banker that this describes every major demonstrable public health success of recent times, such as car seatbelts or the smoking ban indoors, it doesn't show.
The Banker continued, "this is how I am approaching public health in my role as Health Secretary - a deeply pragmatic approach that empowers adults and better protects children".
It feels as if this is part of an attempt to politicise health and prevention, as the smart Richard Sloggett of Future Health (and Alan's former SpAd) observed.
Choice for Labour is does it dodge the issue (likely and as they have done to date) or lean in and make the strong and evidence based counter argument as part of its strong prevention focus (less likely)
— Richard Sloggett (@rcsloggett) June 27, 2023
My take is that Labour don't need to engage with this. We are at the point where the Government’s positions on a wide range of public policy issues credibility-wise don’t actually require detailed opposition policy responses.
‘We’re not them’ is going to do, as the polling data suggests.
That cancer thing
The Government announced a national extension of its programme to catch lung cancer at earlier stages. The first phase of the targeted lung health check scheme by NHS England saw 76% of lung cancers in those tested caught at an earlier stage. It contrasted sharply with news that vital research co-ordinator the National Cancer Research Institute is to close.
Wow. UK's National Cancer Research Institute is to closedown after more than 20 years over concerns about its funding. I am told this infrastructure is vital to cancer clinical trials across UK.
— Shaun Lintern (@ShaunLintern) June 26, 2023
Letter today from NCRI chair: pic.twitter.com/7ZGknDq4HV
InquiryWatch
You may not recognise him on account of the comedy mustachio he's borrowed from Mr Spud, but his name is Selbie, Duncan Selbie.
— Paul Nuki (@PaulNuki) June 29, 2023
He's the former CEO of Public Health England and is viewed by DHSC as one of the most dangerous men ever to have walked the corridors of Whitehall.
Kings Fund report
The new Kings Fund report by the excellent Siva Anandaciva asks the titular question 'How does the NHS compare to the health care systems of other countries?'
The unsurprising answer is 'not well'. People are less likely to survive treatable conditions, such as breast cancer and stroke, than those in other rich nations, the report finds: it suggests that the the problem may be directly linked to the performance of the NHS.
Below-average spending on the health service led to fewer staff and equipment than systems elsewhere: the NHS “trails behind” comparable Western countries’ health systems in its levels of doctors, nurses, beds and equipment, and its performance is “middling at best”.
Crucially, it again confirms that UK patients outcomes from care are worse than those in many other comparable countries on measures including cancer survival rates and life expectancy.
It identifies “strikingly low levels” of such vital clinical professionals as doctors and nurses (as well as lower spending on buildings and equipment, compared with other countries). The UK has three doctors per 1,000 people; Greece has double this number, with 6.3 doctors per 1,000 people.
The UK also has the lowest number of CT and MRI scanners per person (the US has five times as many scanners per person; Germany four times as many).
The economic history of the report is notable: it was commissioned by the Association of British Pharmaceutical Industries.
NadWatch
It does not cost taxpayers £500,000 to train a doctor.
— Andy Cowper (@HPIAndyCowper) June 27, 2023
The Right Honourable Nadine Dorries MP (pro tem) is quite simply lying and making shit up here: https://t.co/1WGmu6N8uL https://t.co/SAYpdTnCHl
I'm not going to make a habit out of this. She is far too many sandwiches short of a picnic, but The People's Nadine made truly special interventions in this Mail piece.
Firstly, the Rt Hon Nadine Dorries MP (pro tem) asserts that it costs taxpayers £500,000 to train a doctor. This figure has long been disproven by evidence and facts, and the real cost to the taxpayer is about £163,000. This is sufficiently well-known that it is fair to accuse former health minister Ms Dorries of lying; making shit up; or both.
Our Nadine goes on to say of the above-mentioned Kings Fund report that "our NHS has some of the worst health outcomes out of 19 wealthy nations compared in an international study.
"The shameful findings ... reveal that we are the worst at saving the lives of those who suffer strokes, the second worst at saving heart attack victims and we significantly under-perform on cancer — which, in turn, has a devastating impact on life expectancy.
"We have the second worst mortality rate overall out of the 19 nations — only the U.S is below us". Mmmmmm. Conservative MP Nadine Dorries will be furious when she finds out which political party has overseen the decline of the NHS and of general population health and longevity over the past 13 years.
Her beautiful claim that "Boris's important social-care reforms have also been quietly killed off by the new administration" rather ignores the fact that these were only going to be funded because the current PM and then-Chancellor Rishi 'The Brand' Sunak insisted on introducing the NHS Levy, which The Truss Supremacy took off the table.
But we reach Peak Dorries with her claim that "one of the hardest nuts to crack to improve performance is the so-called NHS workforce plan, which determines the number of medical school places and nurses and doctors required to keep the NHS functioning in the way we expect.
"The plan has been a thorny issue for many years but was one Boris championed and made an absolute priority in the Department of Health". In the real world, Mr Johnson did not champion an NHS workforce plan and it was not made an absolute priority in the DHBSC.
EveryGrifter
In her first book, Dr Julia Grace Patterson, founder of EveryDoctor and fierce advocate for the future of the NHS, lays bare the truth about the current state of our healthcare system and sets forth transformational ideas on how we could save it.
— Mudlark (@mudlarkbooks) June 29, 2023
The replies to this are golden.
Recommended and required reading
The great Dr Phil Hammond's BBC Radio Four programme, 'How I Ruined Medicine', is broadcast at 8 pm on July 8 on, well, BBC Radio 4. It's bound to be excellent: put your diary note in now.
Ther equally great Dr Kevin Fong will interrogate the current challenges facing the NHS and consider suggested solutions on 10 July on BBC Radio 4, with his four-part documentary series 'The NHS: Who Cares?'. It's bound to be excellent: put your diary note in now.
'Broken Trust: Making Patient Safety More Than Just A Promise', the new report from The Parliamentary Health Service Ombudsman, says that an NHS “culture of cover-up” is leading to avoidable deaths, with hospitals unable to learn from their mistakes. It describes a “defensive and insensitive” culture when patients or their family seek answers following medical errors, with hospitals “routinely” failing to accept their errors. The Ombudsman found four broad causes of preventable physical harm to patients: failures to make the right diagnosis; delays in treatment; poor handovers between clinicians; and failure to listen to patients’ or their families' concerns.
BT's 999 call system crashed, and they don't know why.
Times interview with Wes Streeting
Guardian report on analysis by the Migration Observatory at the University of Oxford which found that the demand for foreign staff had left the NHS and care homes open to “vulnerabilities” including “exposure to international competition for health workers and risks of exploitation”.
Guardian also reports that Rishi Sunak’s government placed a record number of blocks on freedom of information requests in its first three months
Powerful piece on the Priory Group and the weakess of PFD orders.
FT piece on the return of the in-office doctor


