Cowper’s Cut 384: The One After The NHS Ten-Year Plan Dropped

Reactions to the NHS Ten-Year Plan might best be described as studiedly polite from organisations who have or want contracts with the Department For Health But Social Care, and sceptical-to-damning from almost everybody else.
Some that stood out for me were those from actual AI expert Dr Jess Morley; the great Nick Timmins for the Institute For Government; the shrewd Sam Freedman; a broadly positive take from Craig Nikolik on BlueSky; Anita Charlsworth on the unresolved financial issues outed; and this important take from Charlotte Augst.
The Dash Review of patient safety
Well, at least this one didn’t have multiple changes of lead author(s), I guess. Abolition-prone NHS England’s chair Dr Penny Dash this week published her review of patient safety, which will lead to a consolidation in the landscape.
Good: that’s probably necessary. The system that has accreted is a bit of a mess with conufused responsibility, and without obvious effectiveness.
Which was probably part of the intention. In the same way that Simon Stevens-era NHS England accrued vastly increased responsibilities over time because Simon rightly kept pointing out that he wasn’t legally accountable for workforce planning/provider oversight/digital (and ministers and Treasury wanted him to be), it has greatly suited our post-Hunt Health Secretaries to have fairly woolly accountability for patient safety in the English NHS, which as mental health, A&E and maternity all consistently show, is not in tip-top shape.
The Dash Safety Review is a long document, and has picked winners, which is an insidiously tempting sort of thing to do when you decide you are in rationalising mode. It seems broadly sensible, but I am struck by powerful challenges that I have heard from medics and public health leaders.
Their main point is that the Dash Safety Review conflates avoidable deaths caused by a failing health system with avoidable deaths caused by negligence and/or errors in care. This gravely undermines its ‘call to action’ asking readers to consider how many deaths would be avoided if the English NHS were in the top decile of national health system performance.
This is silly: it ignores the OECD data showing that over a relevant period of the past generation, we are mid-table among developed peer economies for spend as GDP per capita, and have significantly fewer hospitals beds per capita.
The Review’s discussion about how the English NHS spends significant sums on patient safety but does not get better overall clinical outcomes is made from a perspective which appears not to acknowledge how much of the time UK medical teams spend firefighting to deliver adequate care because of lack of management capacity and capability to oversee patient flow; as well as to mitigate or work around problems caused by longstanding poor estates and maintenance.
That is a pertinent and large flaw.
The principle of a 29% pay demand
What a difference adequate leadership makes, as the BMA resident doctors’ committee is again showing.
I wrote about their basic errors in media approach when they were calling their new strike ballot. On a low turnout of 55%, 90% voted to enable strike action over the next six months, and the leadership called a first five-day full walk-out strike from 25-30 July.
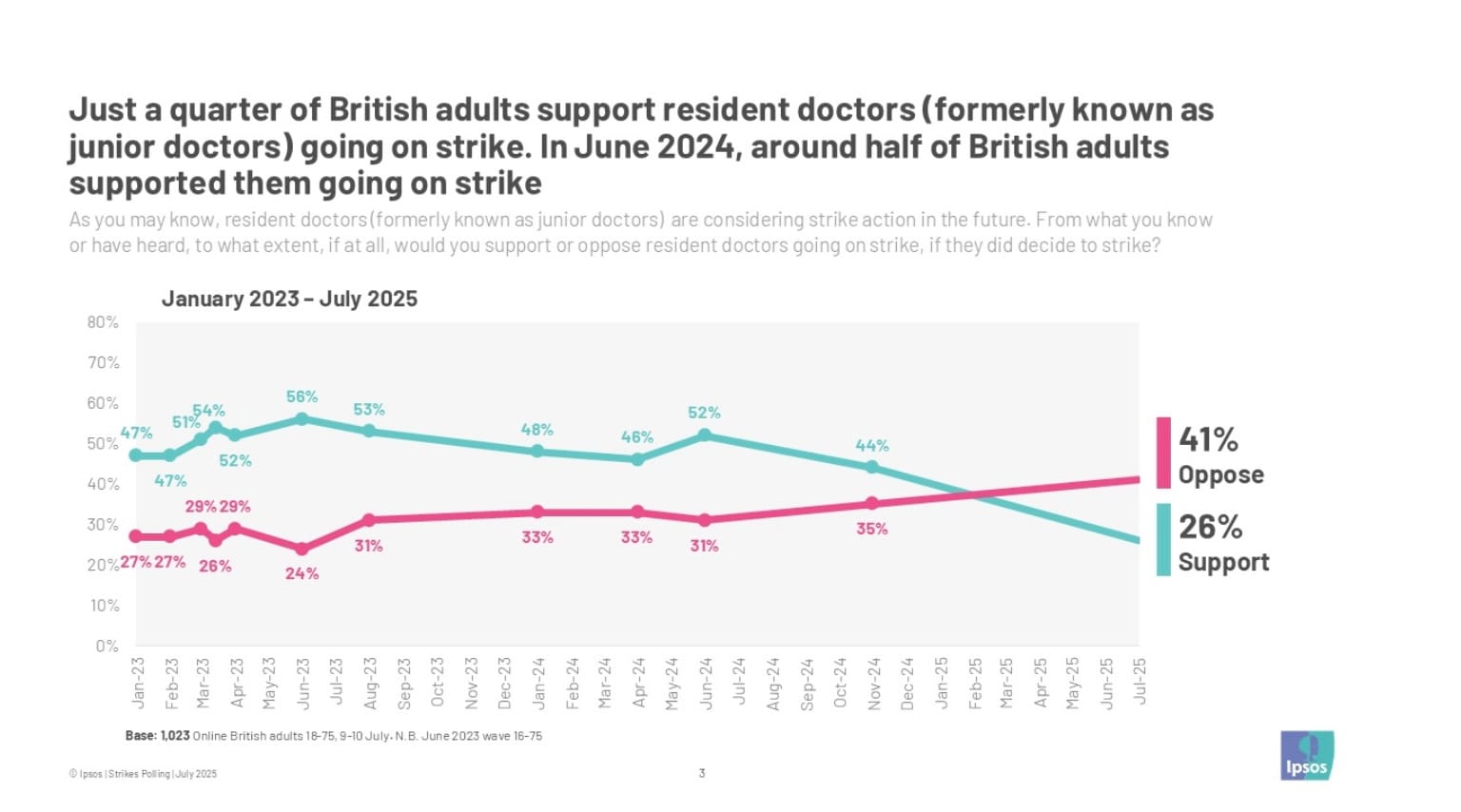
I also wrote at that time thast new YouGov polling found “39% in favour of the possible action, and 48% against it. It’s worth remembering that as Ipsos polling from June 2024 showed, the junior doctors (as they were then known) retained a margin of public support during their long campaign of strikes until the very end, when the Sunak government was given its P45. Ipsos polling also showed a decline in support for striking doctors by February 2024.”
More recent polling shared with The Times by the Good Growth Foundation found the same, only more so: “only one in five voters support resident doctors going on strike again, whereas last year more than half the public backed them. The representative survey of 2,054 British adults by the Good Growth Foundation found that 56 per cent of the public oppose resident doctor strikes, with only 21 per cent supporting them”.
And new Ipsos polling, given to The Guardian as an exclusive, confirms the trend: it finds that “just one in four (26%) British adults support resident doctors going on strike, in polling taken since their latest round of industrial action was announced (9-10 July).
“Two in five (41%) Britons say they oppose the strikes, and 24% are neutral, while 2024 Labour voters are divided on resident doctor’s industrial action. 35% of Labour voters say they support resident doctors going on strike, 32% say they oppose and one in four (24%) say they neither support nor oppose. Conservative and Reform UK 2024 voters are clearly opposed (62% and 58% respectively), as are around 4 in 10 Lib Dem voters (43%).”
Ooops.
If BMA resident doctors’ leaders have not worked out quite how badly Health But Social Care Secretary Wes Streeting wants to be seen to tough this one out (and that PM Sir Keir Starmer and Chancellor Rachel Reeves will gladly let him), then they are even more remarkably foolish people than they already seem.
Public opinion is not everything in an industrial dispute about pay, but it’s a lot. Newly-elected, Labour settled the last pay dispute both deliberately, noisily and publicly. This meant that the excellence of the deal that resident doctors then got cut through to public awareness, loud and clear.
When you see new chair of BMA Council Tom Dolphin telling the Grauniad that residents’ 29% demand is not up for negotiation “because it’s based on a principle. If we picked a different number, that wouldn’t achieve the pay restoration. So that’s why it looks inflexible”, he apparently assumes that people who are not resident doctors or their families could conceivably give a fuck about their principle of pay restoration.
This seems to me like an incorrect assumption.
And in an industrial dispute about getting more money, it is very unwise to say that your position is “a principle”, because negotiation is therefore impossible.
Residents’ leaders’ attempt to make a case out of the lost differential with their 2008 earnings is an absolute hiding to nothing. The BMA chose to let their pay differential go for many years: that’s on them.
I suspect that they will be taken aback by the lack of public support, if they go ahead with their planned strike at the end of the month.

Mr Streeting, meanwhile, is playing this one on ‘full reasonable’ mode. For now. Because he knows that the residents’ leadership have miscalculated their hand, and in so doing, played right into his.
Recommended and required reading
I’ve gone on about this one a lot: the Commons Public Accounts Committee’s new report on the government's use of private finance warns that badly-managed PFI contracts are leading to poor quality assets being handed back to the public sector.
Helen Buckingham pointed me to this excellent piece from Geoff Mulgan, about the importance of plumbing in public sector reform.
The Guardian reports that when giving evidence to the Commons science and technology committee on Tuesday, Palantir’s UK lead Louis Moseley asserted that “the accusation that we lack transparency or this is secretive is wrong. I think that BMA has, if I may be frank, chosen ideology over patient interest. I think our software is going to make patient lives better by making their treatment quicker, more effective, and ultimately the healthcare system more efficient”. (Usual COI declaration: I was previously paid for work as a member of Palantir’s UK health advisory panel.)
The Tony Blair Institute’s health team have reached peak triteness with this daft piece about disruptive delivery.
