Cowper’s Cut 378: Management by improvisation

I wanted to give the new regime at what was once NHS England (and before that, the NHS Commissioning Board) time to work out what they need to be doing and how they need to be doing it, before launching into them over mis-steps and acts of unwisdom.
I afforded this same courtesy to The Woman In Black, Amanda Pritchard, at the start of her NHSE tenure: it seems only fair to do so again.

Health Service Journal’s reporting of the board meeting this Thursday rightly focused on the news line of deputy chair Sir Andrew Morris’ publicly questioning whether the proposal to cut integrated care boards’ funding by 50% “may well not be the right number”.
This was followed by a rather more pointed comment from non-executive director, Sir Mark Walport, who said it was “necessary” to cut ICB costs “substantially”, but “it’s quite difficult to do that if you haven’t got a target operating model that you’re making your changes against”.
Well, yes. These are the joys of management by improvisation.
Hey-ho: this is where we are: the Labour Government has been in office for almost a year, and there is still no plan.
It’s welcome to see some actual dissent articulated in the board public meetings, which have all too often been something of a ‘Potemkin village’ exercise versus the private ‘pre-board’ sessions.
NHSE chief executive Sir James Mackey‘s responding comments about the “very complicated operating model we have ended up with” are a cause for concern. ICBs are regional presences: there was nothing complicated about them, other than their duplicative nature with and unclear separation of powers from the regional presences of NHSE.
But the remarkably worrying (and worryingly remarkable) thing was said by NHSE chair Penny Dash, with her comments that “well over half” of ICB chairs and CEOs “have said they are very excited by this description of a future model [the model ICB blueprint]”, which describes their future role as “strategic commissioners”.
“Officials said there was “quite a bit of energy [among ICB leaders] around all this, which you might not have predicted”, and a “real sense of ambition that has been driving this work”.
Erm, what?
You say that a bunch of people facing an incoming tsunami of job losses and budget cuts from the new national leadership are vigorously nodding along with these plans, seeming positive and energised, so that they can be among the survivors of this latest NHS redisorganisation?
Colour me surprised.
As to ICBs becoming “strategic commissioners”, this is really odd. If we have learned one thing about the history of commissioning in the NHS, starting with GP fundholding in 1991, it is that it is much harder in practice than in theory. Relatively few organisations proved to be any good at commissioning, which is doubtless why it keeps being abolished.
The Oxford English Dictionary defines ‘strategic’ as “the identification of long-term or overall aims and interests and the means of achieving them; designed, planned, or conceived to serve a particular purpose or achieve a particular objective”.
ICBs have already shrunk significantly in resource: they are about to shrink much further. Are they about to be good at doing this difficult thing, which keeps getting abolished?
In a national political environment characterised by narrative drift and fortune-cookie policymaking?
Streeting versus the residents
The ballot is open among BMA resident doctor members over possible industrial action over their campaign for full pay restoration. And new ‘Daily Question’ polling by YouGov suggests that from the outset, they do not have public support.

Of those surveyed, 12% ‘strongly supported’ the residents striking over pay and conditions and 27% ‘somewhat supported. 22% ‘somewhat opposed’, and 26% were ‘strongly opposed’.
That is 39% in favour of the possible action, and 48% against it.
It’s worth remembering that as Ipsos polling from June 2024 showed, the junior doctors (as they were then known) retained a margin of public support during their long campaign of strikes until the very end, when the Sunak government was given its P45. Ipsos polling also showed a decline in support for striking doctors by February 2024.
It’s also worth remembering that public support will not be the only factor in deciding how this industrial action goes.
But it is a significant one, once you get into a political row (which NHS pay fights always are). Ongoing rises in inflation are seen at every supermarket shop, and resident doctors’ new leaders’ faith that they will be successfully restored to their relative earnings level from 2008 may well prove to be misplaced.

Health But Social Care Secretary Wes Streeting used an opinion piece in The Times to appeal to resident doctors not to strike, emphasising that “this year, we have increased pay by more than inflation by an average of 5.4 per cent for resident doctors.
“It is the most generous award across the public sector this year — and building on last year’s deal for the previous two years’ pay settlement, this means resident doctors have seen an average rise of 28.9 per cent over three years, thanks to this government.
“The average starting salary for a full-time resident doctor will now be around £38,800, up from around £29,380 in 2022/2023 — an increase of nearly £9,500”.

Melissa Ryan and Ross Nieuwoudt, the new leaders of the BMA represent resident doctors committee, gave Shaun Lintern of the Sunday Times this exclusive interview, in which they threaten that “doctors could co-ordinate strike action across England to cause maximum disruption to the NHS unless the government bows to their demands for a huge increase in pay … doctors were being forced to consider strikes because of the health secretary changing position towards them.
“After two meetings with Wes Streeting in May, they accused him of refusing to commit to any negotiations over pay for resident doctors”.
Mmmmmmmm.
An observation about the media shots that have been used with every single story I’ve yet seen about the resident doctors’ leaders and the proposed industrial action is that they are appalling.
By appalling, I don’t mean that these photos are unflattering.
I mean that if you want the people who pay taxes and vote to believe that you are reasonable people who are not deliberately looking for a fight with the government about pay, then what you 100% don’t do is pose for all your media photos looking pissed off and with your arms folded over your chest.
Which Ryan and Niewouldt have done.
And which the current BMA media advisory people let them do.
Ooops.
I suspect that this evident attitude is not going to land well in the current economic and political environment of the general public. It may gee up fellow BMA/Doctors Vote types, but it is an interesting index of how smartly Robert Laurenson and Vivek Trivedi led the last industrial action, broadly keeping the media (and thus the public) onside.
It’s also interesting to learn that Ryan is from New Zealand and Niewouldt is from South Africa, in the context that one of the major arguments deployed in the last pay dispute was that we needed to prevent resident (then called junior) doctors from quitting the UK for other Anglophone health systems. Irony, innit.
Likewise interesting is the fact from Shaun’s piece that both are self-confessed Doctors’ Vote BMA entryists. And Ryan reveals in the ST piece that she moved to the UK after studying medicine in Italy, describing her experiences “when I started foundation training in 2020 in the UK”. Which was, of course, denying a training place to a UK-trained doctor: an issue highlighted by SOS Streeting in his Times piece as one that the Government is in the process of changing.
If I were advising the current Government on communications strategy, then I think those points might come into play with my briefings of the media.
Cash back
In advance of the Comprehensive Spending Review on 11 June, the Institute for Fiscal Studies published this data analysis and four major questions for the Chancellor.
First of these four questions is ‘how much to spend on health?’
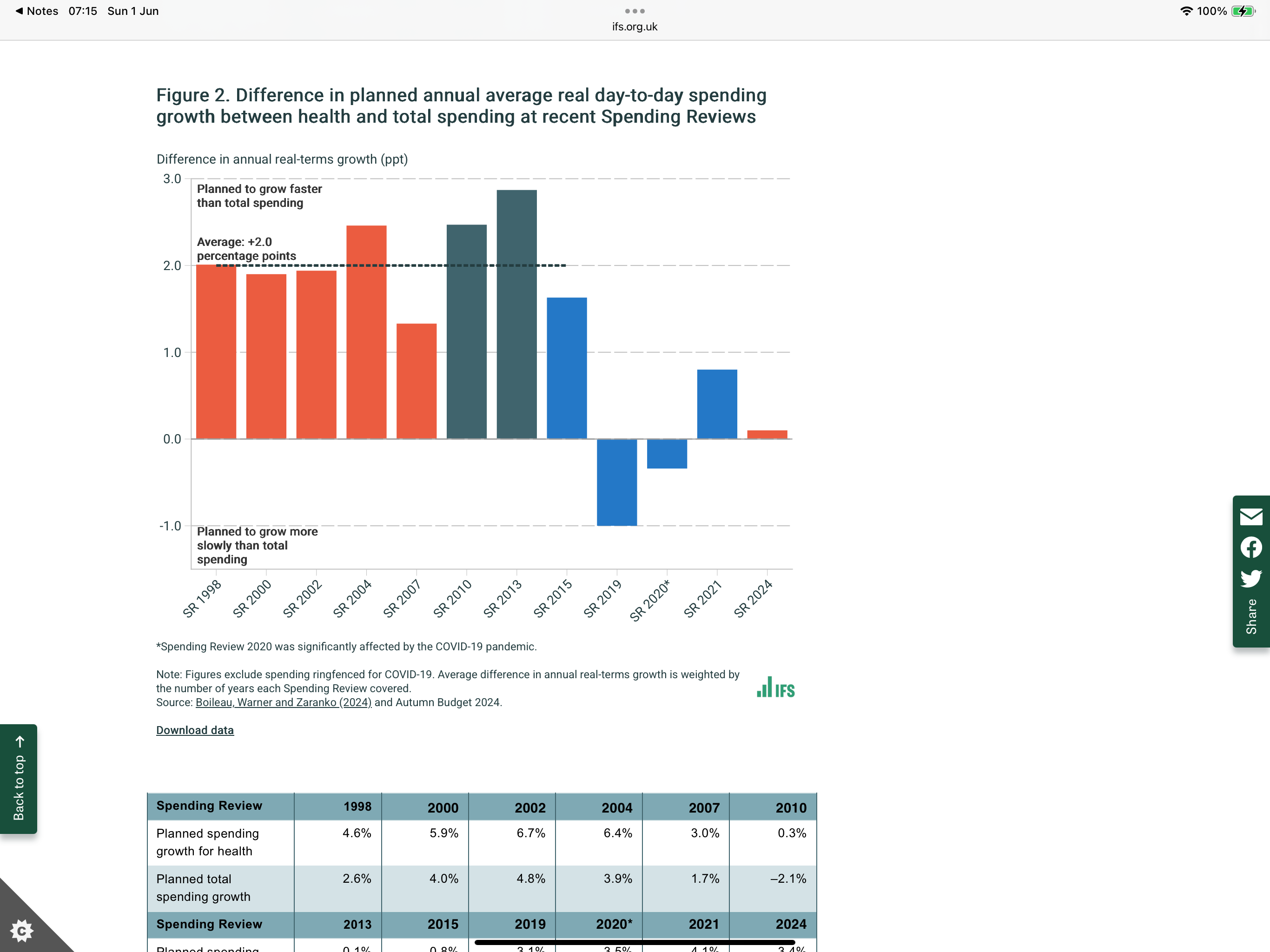
The IFS note the difference in planned annual average real day-to-day spending growth between health and total spending at recent Spending Reviews (see picture above), adding that “importantly, these values represent the difference between health and average growth, not the level of spending growth – as the table below the figure shows, there were large differences in planned total and health spending growth rates over this period”.
Their report concludes that “these scenarios do not set the bounds of what DHSC could receive: even a settlement of 3.4% each year would still be below the long-run average of health spending increases … increasing health funding at anything like the historical average rate (or at anything like the rate we judge to be consistent with the official workforce plan) would mean imposing cuts on other departments to stay within the overall spending envelope.
“Yet increasing health funding by much less could prove incompatible with the government’s ambitions – and the public’s hopes – for meaningful improvements in service performance, even with substantial productivity improvements. This is a central choice for the government at the Spending Review.”

The CSR speculation has been in full flow this week, with the Financial Times reporting that NHS leaders are braced for a rise of 2%.

Contrastingly, The Times reports that the Department For Health But Social Care has been holding out for 4%, with Team 10 Downing Street expected to broker a deal at 3.5%.
The Times also reported on a dispute between DHBSC and the Treasury over which department’s budget should pick up the £1 billion cost of the PM’s pledge to the pharmaceutical industry and to President Trump that the UK will spend more on medicines.
Recommended and required reading
Lib Dem FOI work shared with The Guardian finds that fewer of the English NHS elective operations getting cancelled are now being rescheduled in under 28 days.
Economist Diane Coyle in the FT on what the NHS can learn from Formula One: honestly, much better than it sounds.
Former John Lewis Partnership chair Charlie Mayfield in the FT on his work for the Government supporting people with illnesses to stay in work.
Economist editorial and feature on the NHS. The editorial, which claims that digital is the salvation for everything, gets the size of the pre-Covid RTT backlog wrong: it was 4.4 million, which if it had doubled, would be 8.8 million.
BBC News this week published and broadcast its work on the career of Everybody’s New Favourite Noble Baroness, pandemic profiteer and liar Michelle Mone.
The FT on how robots are now taking on some of the ‘busy work’ at US hospitals.





