Cowper’s Cut 312: History repeating

When @IpsosUK ask people what the most important issue facing the country is the NHS is now number one.
— Keiran Pedley (@keiranpedley) March 2, 2024
Budget this week. Wonder how much we will hear about GP appointments / waiting lists?
We talk about disconnect between political class & voters a lot. Feels big here. https://t.co/3QDqjLQdLp
What most matters about a person or an organisation is never what they say about themselves. (That is PR.)
This doesn’t mean that what people and organisations say about themselves, and how they say it, is unimportant. Choices of language matter: they are often inadvertently psychologically telling. As Ben Johnson wrote, “language most shows a man: speak, that I may see thee”.
What most matters about a person or an organisation is what they consistently do. People who work in opinion polling or market research describe an important differentiation between ‘expressed preference’ and ‘revealed preference’. (This is also why well-designed research often asks you the same question twice, but not sequentially, and always phrased differently.)

I start here because the Government’s plans for imposing the 2024-25 primary care contract funding will increase from the previously-proposed 1.9% to 2.23%, as revealed by Pulse.
Choose strife
This homeopathic increase in the offer clarifies the Government’s revealed preference: to be in an industrial dispute with every major bit of the NHS. The current administration can only have done this because they actually want general practice to join in on England’s year-and-a-bit-so-far of NHS industrial action.
The story adds that “the BMA will ballot the profession on the contract – which has not been agreed – in a referendum to take place from 7 to 27 March, which was postponed … due to the GP Committee pushing for a better deal”. A reduced rate for GPs to join the BMA to take part in this action is reportedly now under discussion. The BMA are not pissing about here.

However, wildly reassuring news is on the horizon: the Government is going to convene a taskforce on the future of General Practice, Health Service Journal reports.
Never mind the Fuller Stocktake, or Jeremy Hunt’s own efforts with the Commons Health Select Committee: both of which date from 2022 - just two years ago.
I don’t think I’ve been as reassured by anything in a long time.
Taskforces always fix everything, immediately. They’re like Commissions, but on steroids.
Iron while the strike’s hot update: send in the SAS!
Specality doctors have just rejected latest government pay deal by 62% to 38%. @RishiSunak said in Jan he'd "reached resolution" with every part of NHS except junior docs. Since then consultants (narrowly) and now speciality docs have rejected that deal. Talks will continue...
— Jim Reed (@jim_reed) March 1, 2024
The results of the SAS (specialist, associate specialist and specialty) doctors’ ballot on the Government’s pay offer were announced this week, and it was a big rejection: by 62% to 38%.
The BMA claims that SAS doctors’ real-terms pay fell by more than a quarter over the last 15 years. The SAS doctors’ committee signalled to ministers that it is willing to continue talks, with a view to the Government putting forward an improved proposal: the body is now launching a survey to consult with members on areas they want to see improvements to the contract offer.
While the SAS committee has not made a call for any industrial action yet, SAS grade doctors (including locally employed ones) have a mandate for taking strike action. This is going to keep on running.

BMA junior doctors committee co-lead Robert Laurenson told The Times that “I don’t think the government wants to end this dispute. I think they are quite happy having the strikes happen. And I think they are failing everyone.
Laurenson also told the paper that SOS Victoria Atkins had “lied” when she promised to bring an improved pay offer back to the table.
The Selbie-Crisp Manoeuvre: NHS England in ‘couldn’t run piss-up in brewery’ shock
To the considerable surprise of absolutely nobody who reads ‘Cowper’s Cut’, the Government’s ongoing backing of Amanda Pritchard into a corner over her job resulted in NHS England doing something counter-productive, stupid and touchingly retro.
As Lawrence Dunhill of Health Service Journal revealed, NHS England this week pulled the classic ‘Selbie-Crisp Manoeuvre’.

HSJ was told that “trust CEOs and chief operating officers have been sent a form to sign, committing to deliver 76 per cent (4-hour A&E target) for the final month of the financial year. It also requests the direct phone number and email of the senior responsible officer.
“Just 13 acute trusts met the (76%) target for January, the latest month for which figures are available. Average performance was 70 per cent, with more than 20 trusts reporting less than 60 per cent.
“Sources from a virtual meeting with NHSE leaders yesterday said chief operating officer Emily Lawson heavily stressed the importance of lifting national performance to 76 per cent this month, saying the target was “very visible” and gives “a signal every day of how well the NHS is doing”. She also said its delivery could impact on how the NHS is funded, and on the levels of confidence in the service, including from staff and patients, according to sources. A repeated narrative of failing targets could also drive poor behaviour, it was suggested.”

Nolan Principles, anybody?
Anybody?
As Ian Higginson, vice-president of the Royal College of Emergency Medicine, promptly observed, this nonsense is “likely to lead to focus on lower acuity patients & pressure on ED folk from management teams. The focus needs to be on exit block not on reputations. That will take long term investment in beds, the workforce, and social / community care”.
Oh dear. Been here before! Didn’t work. Likely to lead to focus on lower acuity patients & pressure on ED folk from management teams. The focus needs to be on exit block not on reputations. That will take long term investment in beds, the workforce, and social / community care. https://t.co/0A2PuemPKn
— Ian Higginson 🌈 (@RCEM_VP) March 1, 2024
Ian is Not Wrong. Indeed, this is the way you’d game the target.
Or you’d just outright cheat. Lose records; declare Opel Four prematurely … put the wrong incentives in place, and a few desperate people will do the wrong things.
2. 76% applies to all Emergency Departments, but this includes Eye Units, Minor Injury Units and Urgent Treatment Centres. I don't care very much if someone waits 4 hours and 5 minutes with a sprained foot, but I get upset if a 85 year old 12 hours on a trolley in a corridor
— Adrian Boyle (@RCEMpresident) March 1, 2024
Adrian Boyle, President of the RCEM, also had his say on Kiss (formerly Twitter): his short thread of observations likewise deserves your attention.
NHS Eng has on many occasions itself said the real cause of the A&E crisis is 'flow' & discharge delays
— Lawrence Dunhill (@LawrenceDunhill) March 2, 2024
This intervention and March push appears to do nothing about that - so it's hard to see it as anything other than purely political in showing Govt it can deliver something https://t.co/FFCuzBzO0w
As HSJ’s Lawrence Dunhill accurately observed on Kiss, “NHS England has on many occasions itself said the real cause of the A&E crisis is 'flow' and discharge delays.
History repeating
This is all just a little bit of history repeating.
2006, to be precise.
Old hands will remember the Selbie Letter, in which Duncan Selbie wrote a formal warning to strategic health authority chief executives about the need to deliver financial balance.
Duncan Selbie’s letter to SHA chief executives on Month 10 Finances (yes, January 2006), required “a plan to materially improve the position for M11 and M12 ... to cover arrangements for a balance sheet review ... the delivery of a surplus from organisations forecasting balance, and a forensic immediate grip on avoiding all discretionary spend by everyone”.
That letter also warned that “Sir Nigel is taking a direct and personal interest in how each PCT and NHS trust leader responds and he will be using the Month 11 FIMS returns in making a judgement on this”.
Ahem.

It is a sign of the utter failure of NHS England’s management and leadership to be explicitly threatening people over hitting targets (be they on access or finance).
Asking chief executives to sign ‘guarantee’ letters and provide their contact details isn’t menacing or motivating: it’s the pathetic conduct of a failed organisation that deludes itself that this might insulate its senior leadership from getting sacked.
It’s not going to be any more effective in 2024 than it was in 2006.
Oh and if there were any actual purpose to NHS Providers or the NHS Confederation in 2024, then clearly they’d already have pushed back on this on behalf of their members, publicly and hard.
Cue tumbleweed.
70s retro: ABBA meets Who’s Next?
The Government now having effectively made explicit their threat to Amanda Pritchard’s job as chief executive of NHS England, you’d like to think they’d have thought about who’s next.
I suspect that imputes more forethought to this administration than is justified, but let’s pretend. As I wrote in June 2023, when reports first reached me of Number 10’s health advisory staff openly denigrating Ms Pritchard to visitors, Sir Jim Mackey was their preferred option. Their attitude is like Sweden’s greatest musical stars: ABBA (anyone but bloody Amanda).
In the wake (literal and metaphorical) of Ms Pritchard’s atrocious 2023 NHS Confed speech, I wrote “Mr Barclay clearly doesn't rate her; nor does the Sunak 10 Downing Street operation: they openly discuss this, and say how much they'd prefer Sir Jim Mackey.
“So, expect briefings against Ms Pritchard to start over the late summer, and to rise in frequency and venom through the autumn. She'll probably be left in place to carry the can for what seems set to be another appalling winter; and set free in the spring due to winter and backlog issues.”
There was and is a problem with Number 10’s preferred option: Jim blatantly hated his spell as interim chief executive of NHS Improvement. In part, he’s not a big fan of living away from his native north-east. No shame in that.
However, for the national job, Number 10 would want their person on hand, to be shouted at in real life. Zoom or Teams just don’t cut it for the serious shouting, apparently.

Moreover, Jim has since been anointed King Of The North-East, with his long-coveted CE job in Newcastle.
So who else is there?
NHSE director of [cough] strategy Chris Hopson would love to think that Chris Hopson’s in with a shout. Nobody else does, though.
So the likely-ish options from the NHSE senior management team would be the chief operating officer-ish duo of long-time interim COO Emily Lawson (well-networked in Number 10 from her secondment there, and from the Covid19 vaccines rollout), and deputy COO Sarah-Jane Marsh.
I am not advocating for their selection, but neither of them is in bad odour with the Number 10 operation. One would also hope that both of these women know a hospital pass when they see one. But who knows? Ambition is a curious beast. Ms Pritchard was not deterred.

“Given the scale of the backlog, there's insufficient time to deliver a meaningful performance recovery before the latest possible date for the next General Election.”
New IFS report on waiting lists and times

The Institute for Fiscal Studies’ increasingly impressive work on health continues with their latest report on ‘The Past And Future Of NHS Waiting Lists In England’. This report won’t tell ‘Cut’ readers much that you don’t already know, but it usefully complies key facts and updates past predictions.
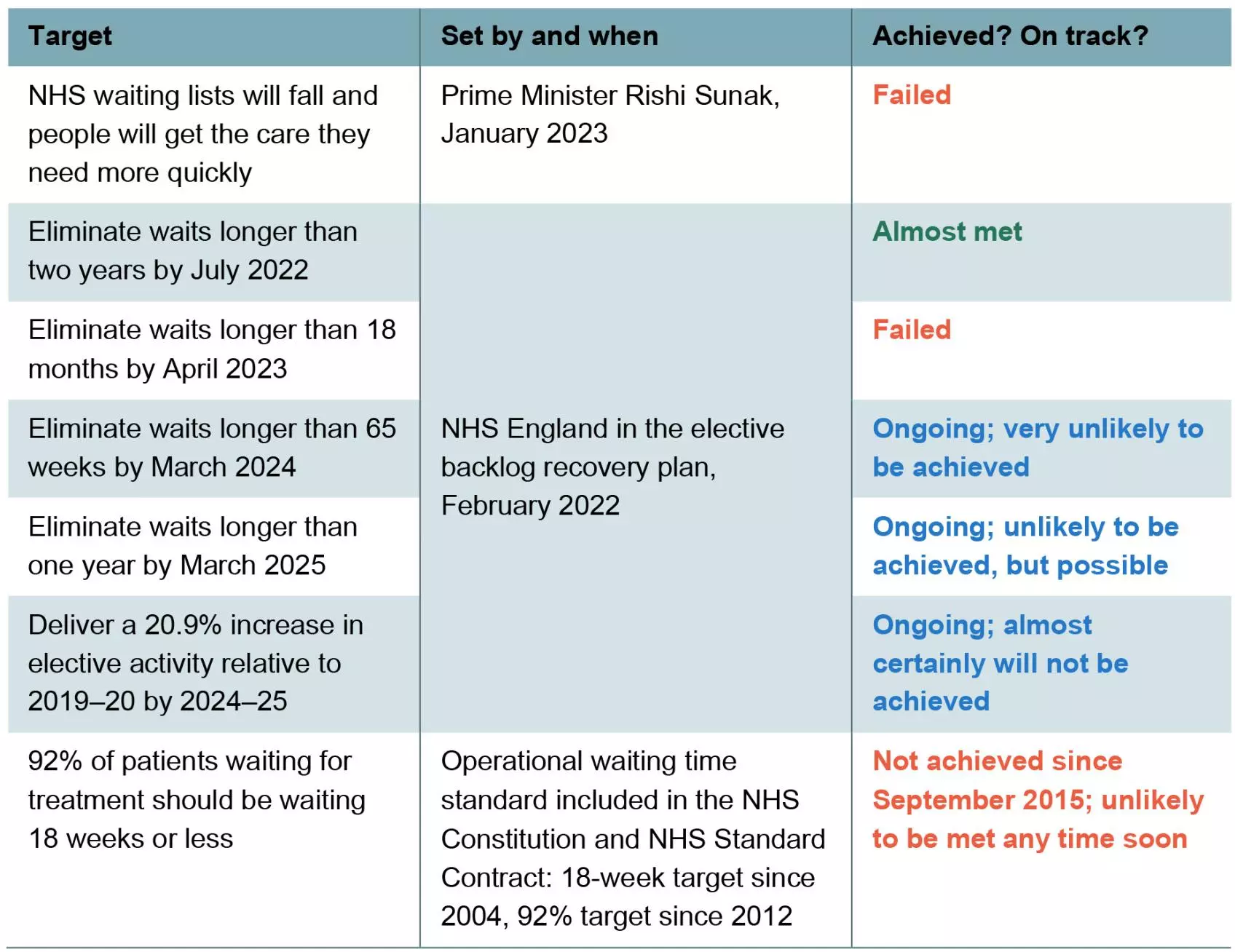
Among its key points (which I’ve abridged) are:
“The NHS elective waiting list in England (already growing pre-pandemic) doubled in a decade, from 2.3 million ‘incomplete pathways’ (patient referred but waiting for treatment) in January 2010 to 4.6 million in December 2019.
“Waiting times also increased over this period, particularly the longest waits. The median waiting times for an inpatient treatment increased slightly from 9.2 weeks in January 2010 to 9.6 weeks in December 2019, while the 95th percentile waiting time for an inpatient treatment increased from 23 weeks to 38 weeks over the same period.
“The elective waiting list grew rapidly during the pandemic, peaking at 7.8 million in September 2023. There are now some signs of hope, with the waiting list falling for three consecutive months at the end of 2023 to 7.6 million in December. This is partly reflecting seasonal trends (pre-pandemic, the waiting list also tended to fall in winter), but also shows that the NHS successfully increased treatment volumes to above pre-pandemic levels in recent months.
“The NHS and government failed to achieve most of their waiting list and waiting time targets in England since 2010. Targets set out in the elective backlog recovery plan of February 2022 to eliminate waits longer than 65 weeks by March 2024 and to increase treatment volumes to 20.9% above pre-pandemic levels in 2024–25 are almost certainly going to be missed. The longer-running target that 92% of patients should receive treatment within 18 weeks of referral has not been met since September 2015, and looks unlikely to be met soon.
“Other NHS waiting lists and waiting times were also rising before the pandemic and have risen even faster since it started. In September 2023, 26% of cancer patients waited longer than two weeks from a GP urgent referral to their first consultant appointment, for example, compared with 8% in December 2019 and 4% in December 2009.
“There is a lot of uncertainty over what could happen to waiting lists in England in the coming years, and so it makes sense to consider a range of scenarios. In the central scenario that we judge most likely, waiting lists would start to fall consistently but slowly from the middle of 2024. But even by December 2027, the waiting list would still stand at 6.5 million in this scenario, remaining far above pre-pandemic levels.
“In our more pessimistic scenario, in which NHS treatment volumes grow more slowly, waiting lists would remain at roughly their current (elevated) level in the years ahead. In our more optimistic scenario, in which the NHS manages to increase treatment volumes at a faster rate, waiting lists could fall more quickly and reach 5.2 million by December 2027 (still above pre-pandemic levels). We therefore assess it to be very unlikely that waiting lists will reach pre-pandemic levels over the next four years.”
I’ve quoted a large chunk of its text here, but it really is worth your time to read the whole document. It is powerful because it is fair and factual.
Its conclusions are important: “the task of getting the waiting list back to pre-pandemic levels could require more than one parliament … the numbers waiting a very long time for treatment have not come down as intended, and NHS hospitals have struggled to increase treatment volumes by anything like the required amount in the period since the plan was published.
“If it were not for the fact that the number of patients joining the waiting list has stayed surprisingly low – a puzzle and a concern in and of itself – the waiting list would have climbed even higher.
“If bringing down waiting lists quickly is a priority, then the next government will very likely need to dedicate additional funding to the health service. In a tight fiscal environment, that will pose challenges and could require some eye-wateringly tough choices elsewhere.
“Funding is also not the be-all and end-all. It is difficult to see any path to a meaningful reduction in waiting lists that does not include a substantial increase in NHS productivity. Finding ways to achieve that ought to be a policy priority, whoever triumphs in the general election.” Amen.
And if you need any other reminders of the objectively awful decline in NHS performance, may I again refer you to Carl Baker’s excellent publication on NHS performance data from November 2023 for the House of Commons Library.
And how is the NHS’s performance ambition?

Well, this week, HSJ’s Henry Anderson disclosed that “systems will be asked to deliver the same amount of elective activity next year as they were tasked with completing in 2023-24 … local leaders have been issued with varying interim targets for 2024-25 that produce an average national threshold of 7 per cent more activity than pre-covid levels, on a value-weighted basis.
“It means the target for the current year has effectively been rolled over into next, suggesting the elective recovery is a year behind schedule. Even if systems hit their thresholds next year, they will still fall well short of the central target set out in the elective recovery plan in 2022”.
Ooops.
Capital punishment

HSJ’s Henry Anderson has this cracking story which reveals that “capital budgets have been raided by almost £1 billion to fund day-to-day cost pressures, including unfunded pay rises and industrial action costs” in the NHS in England.
Henry cites supplementary estimates showing that “around £900 million has been transferred from health infrastructure budgets to cover revenue spending during 2023-24. This includes £200m from the “40 new hospitals” programme”.
Ooops.
As Henry rightly notes, this policy trompe l’oeil “marks a return to the previous decade, when capital-to-revenue transfers became routine and sparked serious concerns from the National Audit Office and other experts. Last summer, Shona Dunn, second in charge at the Department of Health and Social Care, said capital raids were “not something that we would want to do as part of normal financial management” and “certainly not something that we now do”.
“Julian Kelly, NHS England’s chief finance officer, told the same parliamentary committee: “As we are sat here today, we are absolutely seeking to maintain the increase in investment in capital”.”
Capital to revenue transfers? What could conceivably continue to go wrong?
Thirteen more going to RAAC and ruin
In a remarkable piece of cosmic irony, this week also saw HSJ’s Zoe Tidman update us that thirteen English NHS hospitals have revealed that, having previously declared themselves to be reinforced autoclaves aerated concrete-free zones, they are in fact RAACed with this fast-decaying cheap building material.
The Department For Health But Social Care’s updated official list of NHS buildings with known RAAC now numbers 54.
Ooops.
The Alan comeuppance

I’m sure that you’re as disappointed as I am by the failure of Everybody’s New Favourite Noble Baroness, Tory peer and liar Michelle Mone to enliven the health policy nation with further shenanigans this week. It’s a simple lack of effort, Baroness Mone, and it won’t do. We require far more from our court jesters.
Thank goodness, then, for the ever-reliable People’s Partridge himself, Mr Matthew Hancock, returning to trouble our consciousness like a fart in a spacesuit.
The Times’ Patrick Kidd reports Alan’s appearance at Slough’s top comprehensive school Eton, making a speech to pupils. So far, so on brand: he’s obviously not picking up the sweet TikTok influencer gigs yet.
The Paper Of Record informs us that The People’s Partridge began his talk with a joke about how Sir Jacob Rees-Mogg “is not a good politician”. Alan The Arbiter? Pot-kettle-black?
Alan’s latest comeuppance came in the Q&A after his speech: “a thin bespectacled lad called Peter immediately strode out to the wicket and declared that his father was a great man in public and in private. “Especially,” Rees-Mogg Minor added, “as he remained loyal to his wife”.” This filial defence was reportedly met with uproarious applause.
Recommended and required reading
New Institute For Government report suggests there's a need to restore standards in public life. Can't think why ...
Financial Times Budget preview/scene-setter
Policy Exchange’s latest report suggests that workplaces have a role to play in improving the population’s health.
My latest column for Pharmaceutical Journal.
Another fine ‘Mythbuster’ from Steve Black in HSJ.
Lancet article reviews international experiences of provider privatisation, and shows with evidence that they do not work.
Inadvertently hilarious Mail article suggesting that a possible £36 million a year cost of ill-defined ‘health tourism’ to the English NHS (current annual revenue budget: c. £160 billion) is in some way catastrophic.
A brilliant example of frugal innovation.
Depressing Guardian piece about violence against NHS staff.
The UK Recovery programme’s funding from the Government ends this week (it’s continuing thanks to some US philanthropists).
Julian Patterson’s latest HSJ column is magnificent.
Shadow Health Secretary Wes Streeting makes a fair point in the Boris Johnson Fanzine on ‘crackers’ NHS language: “when people read that the NHS has done daft things, like remove any language referring specifically to women from NHS documents in the name of inclusion … This is clearly crackers, and it should not be happening.
“We’ve also got to bear in mind that black women are four times more likely to die in childbirth than white women, black men are twice as likely to die from prostate cancer than white men. And when it comes to a very common condition like endometriosis, women are waiting more than seven years for diagnosis.
“So that’s why I want the diversity and equality focus to be on how we tackle those health inequalities, not whether people are being right on and doing daft things – well-meaning things – in the name of diversity and inclusion.”